Canine Hip Dysplasia Part VII - Surgical Management of Canine Hip Dysplasia
Canine Hip Dysplasia Part VII Surgical Management of Canine Hip Dysplasia
Surgery may be recommended for suitable candidates, taking into account expected activity level, longevity and use and value of the dog.
This article is the seventh in an eight-part series on canine hip dysplasia (CHD). What follows is written from the perspective that the readers are serious and conscientious breeders who are the guardians of the genetic pools that constitute their breeds. While this series of articles will not replace a stack of veterinary and medical texts, it is a relatively in-depth look at the whole problem of canine hip dysplasia. Furthermore, the series is designed to be retained as a reference. When you finish reading this series, you will have a sufficient background to make rational breeding choices and will be able to discuss the subject from an informed basis with your veterinarian. You may not like what you read, but you will be more competent to deal with the problem.
Conclusions from part I:
Genetics is the foremost causative factor of canine hip dysplasia. Without the genes necessary to transmit this degenerative disease, there is no disease. Hip dysplasia is not something a dog gets; it is either genetically dysplastic or it is not. An affected animal can exhibit a wide range of phenotypes, all the way from normal to severely dysplastic and functionally crippled. Hip dysplasia is genetically inherited.
Conclusions from part II:
While environmental effects, to include nutrition and exercise, may play a part in mitigating or delaying the onset of clinical signs and clinical symptoms, hip dysplasia remains a genetically transmitted disease. Only by rigorous genetic selection will the incidence rate be reduced. In the meantime, it makes sense to have lean puppies and to avoid breeding animals from litters that showed signs of hip dysplasia. It is probable that even normal exercise levels may increase the phenotypic expression of CHD of a genetically predisposed dog. Stay away from calcium supplementation of any kind; all it can do is hurt. There is no conclusive evidence that vitamin C can prevent hip dysplasia, but there is some evidence that vitamin C may be useful in reducing pain and inflammation in the dysplastic dog. Fortunately, large doses of vitamin C are readily excreted, but it is still possible to cause untoward side effects with megadoses.
Conclusions from part III:
Canine hip dysplasia can be difficult to diagnose, as a number of other orthopedic neurological, autoimmune and metabolic problems may mimic it. Controversy surrounds the question of positioning for hip X-rays and what part joint laxity plays in hip dysplasia. Hip dysplasia may be more common in large and giant breeds and is one of the most over-diagnosed and misdiagnosed conditions.
Conclusions from part IV:
Sadly, no breed registry in the United States requires genetic screening of parents as a prerequisite for litter registration or even offers a "fitness for breeding" certification. The current registries for hip dysplasia (and other genetically transmitted problems) cover so little of the American Kennel Club-registered dog population that their impact so far has been minimal. The tools we need are there. Joint responsibility for failing to use the tools at hand lies with the AKC, United Kennel Club, parent clubs and individual breeders.
Conclusions from part V:
The two major methods of diagnosing canine hip dysplasia available to the fancy in the United States are those followed by OFA and those followed by PennHIP. Both are diagnostic; however, the hip-extended protocol followed by OFA may produce false-negative results. The protocol followed by PennHIP has a prognostic or predictive capacity through the use of statistics and a carefully guarded data base that allows a prediction to be made with respect to the probability of phenotypic expression of canine hip dysplasia. No one has a clear quantification of the gray area between obviously clear and obviously dysplastic hips.
Conclusions from part VI:
For many animals, canine hip dysplasia is a manageable condition, and they can lead relatively normal and active lives given that caution is exercised. Every dog is different in its response to pain and the treatment protocol needs to be tailored specifically to the particular animal. Only aspirin and phenylbutazone ("bute") are FDA-approved drugs for use in dogs, but they are not without serious side effects. Corticosteroids are dangerous and may require experimenting to find proper dosage levels and intervals. Favorable results have been reported from chiropractic, physical drug and nutritional therapy.
It is no accident that this discussion of surgical interventions should appear at the end of this series on hip dysplasia, as it is not only the viewpoint of the authors but also many veterinarians that these procedures are measures of last resort. On the other hand there are very clear indications for surgery.
Surgery is indicated when:
- medical management has resulted in unacceptable side effects;
- medical management has not been effective in restoring function and eliminating pain;
- surgery will correct current problems;
- surgery will preclude or ameliorate future problems.
It is important to remember from the earlier articles in this series that canine hip dysplasia, as a degenerative joint disease, is a process, and that different interventions may be required at different stages in the process.
Many animals lead a non-working pet life and have a level of activity that would not be expected to accelerate the degenerative process. Thus they might not require surgery in order to sustain that level of activity for their remaining life spans. Working and other high-activity-level dogs are another issue entirely, as are dogs used for special purposes. Some of these procedures are also recommended when there exists a genetic or traumatic orthopedic condition that must be corrected in order to begin long-term medical treatment modalities.
We should also note that surgery is used jointly with adjunct therapies.1 Weight control, or where indicated weight loss, along with appropriate exercise restrictions, also apply. Careful consideration must be taken to limit the post-surgical canine patient to those exercises and exercise levels that do not accelerate the degenerative process. Water exercise is ideal as a non-weight-bearing activity that prevents atrophy of those muscle masses that support the hip, burns calories and maintains cardiovascular fitness. For those dogs for whom water activities are not available, or who do not enjoy the water or retrieving, the choice of exercise surface should be considered. Hard-packed sand along the water’s edge, soft grass or dirt roads and trails are much preferred over concrete or asphalt. Appropriate drug and nutritional support are also indicated.2
Surgical procedures for the management of canine hip dysplasia tend to be controversial. Each procedure has its pros and cons, and therefore, not surprisingly, there are veterinary orthopedic surgeons who for a given patient would choose different procedures, much as in human medicine. This leads the authors to conclude that there is no one ideal procedure that is suitable for all stages of the disease process. Each dog presenting with hip dysplasia may be more or less a candidate for one or more of the procedures described here. There are, however, clear indications for the type of procedures that might be most beneficial at different stages of the disease process.
 Femoral neck lengthening
Femoral neck lengthening
The goal of this article is to acquaint the reader with the options available, and to provide a depth of understanding sufficient that the reader may participate in the choice of techniques chosen or rejected by the attending veterinary orthopedic surgeon. Caveat: Many orthopedic surgeons become so skilled in one method that their success is greater with that procedure than with another that theoretically might be better suited for the candidate animal. The authors suggest finding a surgeon comfortable with a particular procedure that would seem to fit the case, and whose patients have done well. Be aware that no one procedure is suitable for all candidates for surgery and that some level of argument may be made for and against any given procedure for any given candidate. The best choice, when factoring cost, age value of the animal, use of the animal, stage in the disease process, etc., may not always be clear.
Before the development of advanced degenerative joint disease, surgical options include:
- pectineal myotomy-cutting or dissection of the pectineous muscles;
- pectineal myectomy-excision of a portion of the pectineous muscles;
- three-plane intertrochanteric osteotomy-changing the angle of the femoral head;
- triple pelvic osteotomy-cutting the pelvis into three pieces then putting it back together with more favorable acetabular angles.
After the development of advanced degenerative joint disease, surgical options include:
- excision of the femoral head and neck;
- shelf arthroplasty;
- total hip replacement.
The excision of the femoral head and neck is often selected for those animals in the end stage of the disease. For advanced cases, where the value of the animal warrants the expense, often the procedure of choice is total hip replacement. For those dogs that are too far advanced into degenerative joint disease for a reconstructive procedure such as triple pelvic osteotomy to be effective, and yet not bad enough to warrant total hip replacement, there is a new "shelf" procedure in development that uses a bone graft technique to extend the acetabular rim and improve femoral head coverage. Due to their complexity and cost, we will reserve our treatment of femoral neck and head excision and THA (total hip arthroplasty) to the eighth and final part of this series.
Pectineal Myotomy/Myectomy
Originally developed by J. Barden, Larry J. Wallace, D.V.M., M.S., modified the procedure in 1967 to include the tenectomy (cutting out a portion of the tendon) or tenotomy (cutting of the tendon) of the pectineus tendon of insertion (that part of the muscle that goes into and attaches to the bone). Pectineal myotomy/myectomy was first used to treat canine hip dysplasia in clinically affected dogs.3 Wallace’s procedure is by no means a cure for CHD, but has been described as somewhat effective in temporarily relieving pain and restoring function. One of the adductors of the hip, the pectineal muscle brings the hind leg in toward the mid-line of the dog. The rationale for this procedure is to relieve the tension on the joint capsule, caused by the upward force on the coxofemoral joint from a contracted pectineus muscle. It is also thought that improved weight loading of the femoral head within the acetabulum may result from the increased range of abduction. Note the difference between "adduction" (moving toward the center line) and "abduction" (moving away from the center line). This type of surgery should be considered strictly therapeutic in nature and does little or nothing to stabilize the dysplastic hip. Therefore, the owner of an affected animal can expect the degenerative changes due to osteoarthritis to continue.
Figure 3 (left) shows before and Figure 4 (right) shows after triple pelvic osteotomy and femoral neck lengthening. Figures 1-4 courtesy of Dr. Barclay Slocum, Slocum Veterinary Clinic.
Complications attributed to this surgical option include fibrotic reattachment of the muscle or tendon and seroma formation. Seroma are tumor-like collections of blood and serum in the muscle tissue. A modification of the earlier procedure, which allows suturing the tendon of insertion to the "belly" of the pectineus muscle, has been suggested to address both of these post-surgical consequences.
Published data showing the efficacy of this surgical treatment include several studies where dogs that had had pectineus surgery at 4 to 12 weeks of age demonstrated no beneficial effects from this procedure when evaluated again at 12 to 47 months.4,5 However, this surgery is used in clinical practice when an owner cannot afford one of the more sophisticated surgical procedures, or to restore function to a working animal when the dog needs to be used in the near future. Activity is restricted for only two weeks after this type of surgery.
Shelf Arthroplasty
The purpose of shelf arthroplasty is to form an extension over a shallow acetabulum to improve joint stability. Diminished depth of the acetabulum is most often the result of osteophyte formation. This procedure is supposed to improve coverage of the femoral head, prevent stretching of the joint capsule and thus eliminate and reduce pain. But as yet, there is no evidence that this surgery alters the progression of CHD in young dogs.
Because of the controversy surrounding the BOP (biocompatible osteoconductive polymer) shelf arthroplasty, which questions both the efficacy of the procedure itself and the safety of the material used, the authors choose not to recommend this surgical option. "I have reservations about the procedure," says Dr. Marvin Olmstead, professor of small animal orthopedics at the Department of Veterinary Clinical Sciences, College of Veterinary Medicine, Ohio State University. "When one critically looks at the postoperative radiographs provided by the BOP manufacturer, it is apparent that the arthritis continues. I know of several cases in which there was development of foreign body reactions and draining tracts from this substance." [Authors’ emphasis.]6 Dr. Barclay Slocum of the Slocum Clinic (Eugene, OR) also concurs with this opinion and adds, " It just doesn’t do what it claims to do."7 Minor complications can include broken screws and seroma formation. There are a number of researchers developing bone graft shelf arthroplasty techniques to extend the acetabular rim to provide greater coverage of the femoral head. Shelf arthroplasty is not a true arthroplasty as it does not change the existing joint surfaces, it only extends their rim.
Intertrochanteric Osteotomy
Prior to improvements in the method for performing triple pelvic osteotomy, the intertrochanteric osteotomy was commonly used if there was adequate depth in the acetabulum socket, and if the dorsal rim was normal, i.e., osteophyte formation had not begun.8 This surgery reduces the angle of the femoral neck, which improves congruity between the femoral head and the acetabulum, resulting in an improved fit. Because it corrects conformational and structural problems of the femoral head, this procedure must be performed before any major remodeling of the acetabulum has occurred. Nevertheless, pain and radiographic subluxation must be clinically evident prior to any reconstructive surgery in order to justify the pain, effort and expense. The average angle of inclination of the femoral neck in the dog is 149 degrees(normal range 141 to 157 degrees). The intertrochanteric osteotomy over-corrects this angle to approximately 135 degrees by removing a wedge of bone. See Figure 5 and Figure 6 for before and after images. This is thought to increase the surface area over which the pressure or "load" is spread. The greater the surface area, the less the pressure per unit of area there is on the coxofemoral joint in any one place.
Figure 5 (left) shows before and Figure 6 (right) shows after double intertrochanteric osteotomy. Note the improved congruity between the femoral head and acetabulum. Photos courtesy of Braden, T.D.; Prieur, W.D. "Three plane intertrochanteric osteotomy for treatment of early stage hip dysplasia." Vet Cl N Am Sm Anim Prac. Vol.22 No.3 May 1992. pp.624-643.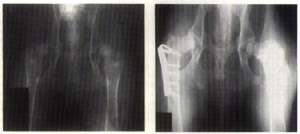
Two studies have been done to evaluate the effectiveness of this surgical procedure. The first one was published in 1987 and assessed 183 dogs from one to seven years after the surgery was performed.9 The results of this study demonstrated an 89.6 percent "excellent" or "good" return to motor activity. "Excellent" was reserved for those dogs that exhibited a normal gait and no pain when exercised over long distances. "Good" was defined as a slight limp appearing after exercise, but exhibiting a normal gait while walking or running. Better results were attained if the dogs were operated on prior to the appearance of degenerative joint disease. Only 12.1 percent of the dogs with severe osteoarthritis had excellent results as opposed to 51.4 percent of those dogs without any osteoarthritis before surgery and 45 percent of those dogs with mild degenerative joint disease. A later study covered the seven-year period between 1980 and 1987. Published in 1990, this article evaluated 37 dogs with a total of 43 hip surgeries.10 The evaluation procedure consisted of a questionnaire and/or an orthopedic examination. Also included was a report from the owners via telephone. A rating of "excellent" in this second study was defined as normal function, whereas "good" was characterized as normal weight-bearing with joint stiffness after strenuous exercise or a long rest. Follow-up consisted of:
- owners’ phone reports-68 percent "excellent" or "good" at 11 months;
- a questionnaire that evaluated dogs at one year-70 percent "excellent" or "good";
- an orthopedic exam at 15 months-80 percent "excellent" or "good."
The stated goal of this procedure is to relieve pain. In humans, the surgery provides relief for an average of five to six years.11 It has been assumed that the results are somewhat similar in dogs, but the actual expected duration of improvement has not yet been determined.
Triple Pelvic Osteotomy
The TPO may be considered the exception to the view that these surgeries are "salvage" in nature. For this procedure to be effective, this surgery must be performed before major remodeling of the femoral head and the acetabular rim has occurred. That means that the primary abnormality should be radiographic indications of subluxation of the affected hip.
Slocum believes there are two forms of canine hip dysplasia.12 One condition exhibits either a shortened femoral neck or an improper angle between the femoral head and the long axis of the femur. This problem can be corrected by lengthening the femoral neck (Figure 1). The femur is split down the long axis and a polymer wedge is placed proximal (toward the center) to the femoral head. The bone is then wired together and the new bone fills in the gap. Some controversy exists with this procedure, however. "I view the femoral neck lengthening procedure with extreme caution," says Dr. Gail Smith of Penn State. "Although I have not performed mechanical testing on femurs treated with this method I estimate the reduction in femoral torsional strength [resistance to twisting] to be at least 70 percent, leaving the femur susceptible to fracture. This procedure has a theoretical basis only, and I am unaware of scientific proof supporting its clinical efficacy."13 In answer to this criticism, Slocum adds, "Although drilling a hole or cutting a bone as in any surgical technique will make a bone weak to torsional stresses, the healed bone is strong, durable and functional. After healing has been completed in the femoral head lengthening, no clinical experiences of this bone fracturing has been reported by other doctors using this technique or experienced by me in my clinical practice."14
By far the most common form of CHD that Slocum sees in his clinical practice is acetabular hip dysplasia.15 This type is characterized by having an excessive slope to the dorsal rim of the acetabulum. When the dog is standing, it is this portion of the pelvis that supports the animal’s weight. Slocum believes excessive slope of the acetabulum is the primary cause of the sideways displacement or subluxation of the femoral head. This leads to stretching of the round ligament, which in turn can cause the joint capsule to stretch, thus producing the hip laxity that commonly characterizes CHD.
Slocum believes that the best candidate for this type of surgery should have a combined dorsal acetabular rim (DAR) slope of more than 15 degrees. The determining factors for suitability of triple pelvic osteotomy are: DAR angle, angle of reduction and angle of subluxation. His past candidates have been from 4 months to 8 years of age. The surgical procedure consists of cutting the pelvis at three different points (Figure 2). This allows the acetabulum to be tilted until it is perpendicular to the femoral head. With the force generated at a 90-degree angle the femoral head is kept within the socket by the weight of the animal. This procedure also relies on muscular contraction to keep the femoral head seated within the socket, so any neurological deficit or muscular problems would necessarily disqualify a dog for this type of surgery. Various methods are used by the surgeons to determine the angle at which to tilt the pelvis. Slocum uses the DAR projection and draws a line parallel to the top of the femur. This indicates the required angle when this line intersects the dorsal slope.
Note that the intertrochanteric osteotomy and the triple pelvic osteotomy are in essence two approaches to the same overall goal: that of aligning the acetabulum and the femoral head for the greatest congruity. The intertrochanteric osteotomy attacks the problem from the pelvis. If done well, indications are that the results are beneficial and similar. Indications for a triple pelvic osteotomy combined with a femoral neck lengthening are: the dorsal acetabular rim is damaged, the acetabulum is not filled with osteophytes and the joint capsule is stretched. Figure 3 and Figure 4 show before and after imaging of femoral neck lengthening and pelvic osteotomy procedures done on the same animal. Note the great improvement in the femoral head to acetabular cup fit in the after view.
Conclusions:
Surgery is a viable option given the suitability of the candidate animal, the financial resources available, the expected activity level, longevity and the use and value of the animal. Choice of intervention, medical, surgical or activity level is process-dependent. Problems with certain procedures may be associated with improper patient selection relative to the stage of the disease. To be fair, patient compliance, i.e., owner post-operative management, may also be a significant factor.
The next and final article in this eight-part series will cover total hip replacement. Exciting new advances have been made and are currently supported by manufacturers. The costs remain high, but then so are the benefits to be gained in a suitable candidate.
References
- Goring, Robert. "Surgical and medical management of canine hip dysplasia." Hoffman-LaRoche Symposium on Degenerative Joint Disease. Orlando, FL January 12, 1992. Pp.7-15.
- Cargill, J.C.; Thorpe-Vargas, S. "Medical management of canine hip dysplasia." Dog World. October 1995. Pp.24-28.
- Wallace, L.J. "Pectineous tenectomy or tenotomy for treating clinical canine hip dysplasia." Vet Clin N Am. 1971. Vol. 1. Pp.455-465.
- Bowen, J.M.; Luis, R.E.; Kneller, S.K., et al. "Progression of hip dysplasia in German Shepherd Dogs after unilateral pectineal myotomy." J Am Vet Med Assoc. 1972. 161:899-904.
- Lust, G.; Craig, P.H.; Ross, G.E.; et al. "Studies on pectineous muscles in canine hip dysplasia." Cornell Vet. 1972. Vol. 62. Pp. 628-645.
- Smith, Carin. "Treatments for hip dysplasia spark controversy." J Am Vet Med Assoc. Vol. 201. No. 2. July 15, 1992.
- Personal communication with Dr. Barclay Slocum, Slocum Clinic, (503) 689-9393. August 17, 1995.
- Prieur, W.D. "Intertrochanteric osteotomy in the dog: Theoretical considerations and operative techniques." J Sm Anim Pract. 28:3-20, 1987.
- Walker, T.; Prieur, W.D. "Intertrochanteric femoral osteotomy." Seminar Vet Med Surg (Small Animal). 2:117-130, 1987.
- Braden, T.D.; Prieur, W.D.; Kaneene, J.B. "Clinical evaluation of intertrochanteric osteotomy for treatment of dogs with early-stage hip dysplasia: 37 cases (1987-1989)." J Am Vet Med Assoc. 196:337-341, 1990.
- Reigstad, A.; Gronmark, T. "Osteoarthritis of the hip treated by intertrochanteric osteotomy." J Bone Joint Surg Am. Vol. 66. Pp. 1-6. 1984.
- Slocum, B.; Slocum, T.D. "Pelvic osteotomy for axial rotation of the actabular segment." Vet Clin N Am. Vol. 22. No. 3. Pp. 645-682. May 1992.
- Smith.
- Personal communication with Dr. Barclay Slocum, Slocum Clinic, (503)689-9393. August 22, 1995.
- Slocum, B; Slocum, T.D.
